In a typical week in my weird world of retrieval medicine, emergency medicine, and intensive care I went from immersive prehospital ECMO simulation on Monday to prescribing an enema for a patient on the ED short stay unit on Thursday who hadn't done a poo for week. Decades of training and multiple exams and EM/critical care fellowships to my name and there I am, a PGY30, not only doing the job of an intern but feeling like one in terms of how little I know (or care) about the management of constipation.
Highlights this week:
Nuts keeping me alive during prehospital sims
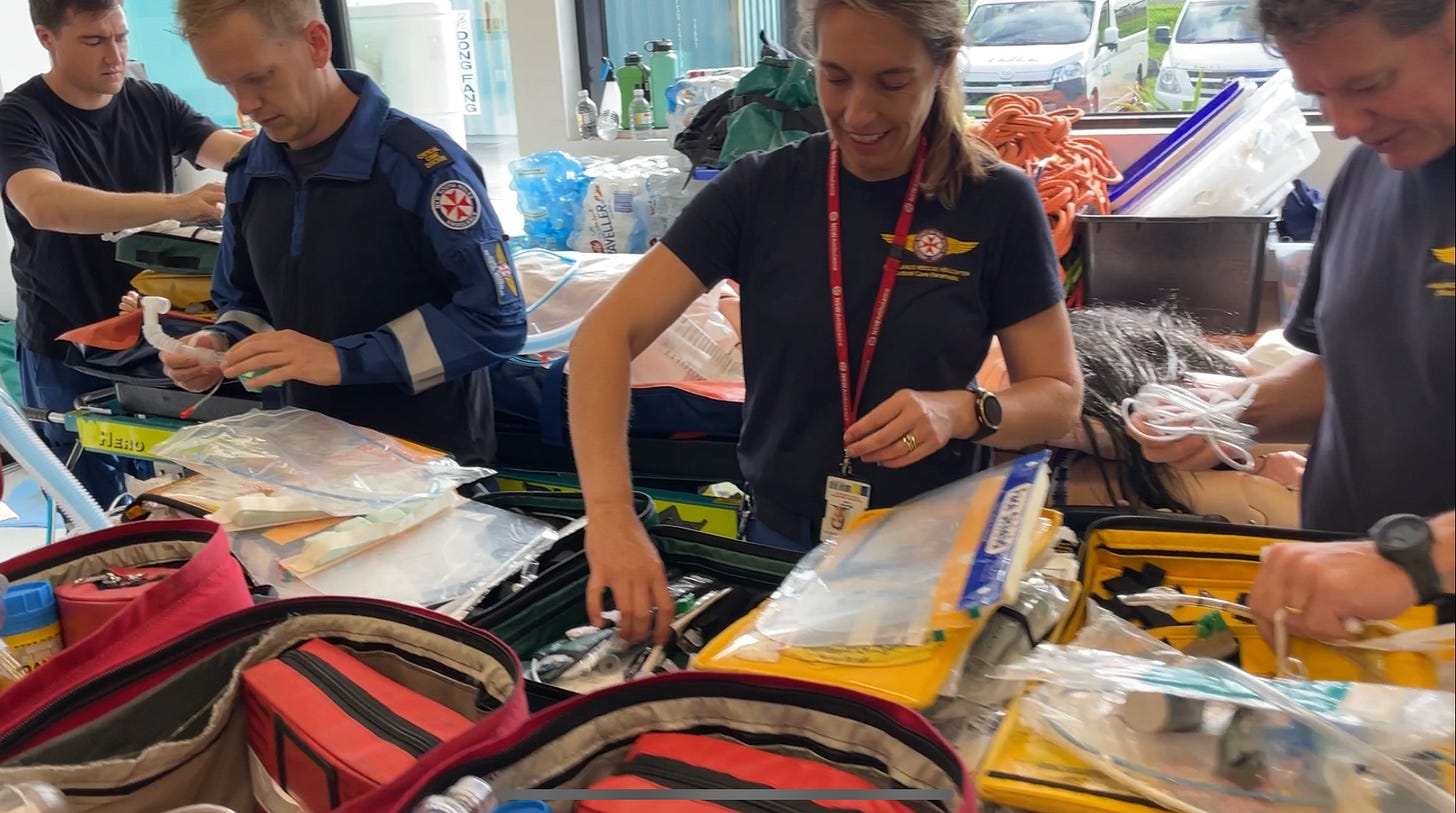
The helpfulness and team spirit of our critical care paramedics and HEMS registrars in preparing training packs for next week’s induction training
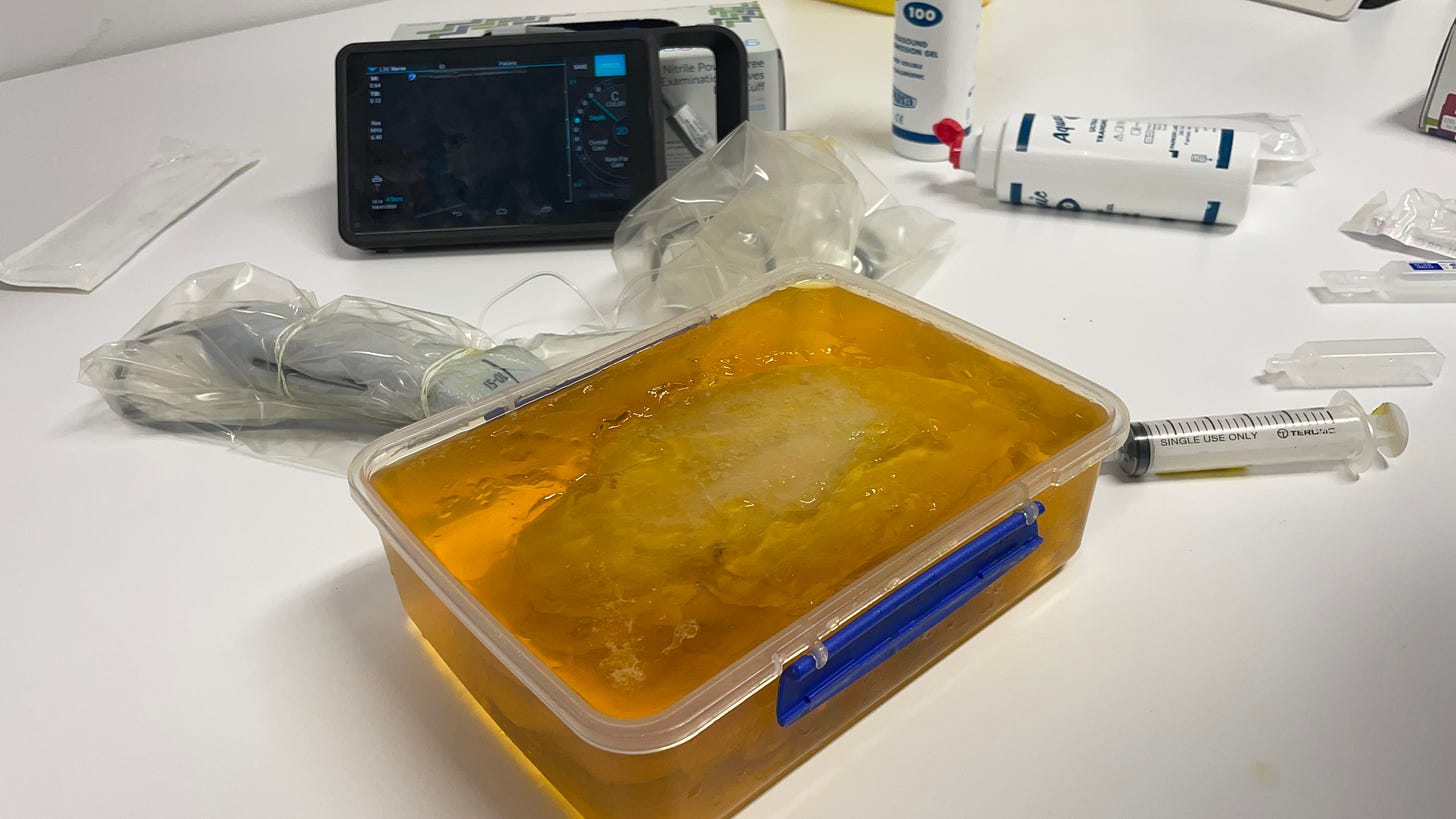
Using an amazing model to teach / practice serratus anterior plane blocks - a procedure we do almost daily in our emergency department
Managing a lady visiting from overseas with an off-ended distal radius fracture. No insurance meant that she couldn’t afford an admission for surgery. The Resus Room was full so we were unable to provide procedural sedation. I decided to do a haematoma block at the fracture site which worked perfectly! The orthopaedic registrar did an impeccable reduction. She’ll be flying home on Sunday with both her discharge instructions and a referral letter in her native language thanks to Google Translate, with the radiographic images on her phone. That was literally the first haemotoma block I’ve done since I moved from the UK 15 years ago, but I’ve done so many in the past it still felt like it’s something I do every day! It was striking how so many staff asked why we don’t always do it like that?
Hypotension Video
Sometimes we’re asked to review a well-looking patient with mild hypotension, and it can be difficult to determine whether it’s a normal blood pressure for them or something we need to do something about. I made a three minute video to make it easy, using the Four W’s of When Not To Worry:
Airway Tip
When using a bougie for intubation, ensure your teams are trained so that the laryngoscopist NEVER takes his/her eyes of the PRIZE! Looking around for the bougie can result in a loss of view, especially with direct laryngoscopy. Make sure the airway assistant is ready to place it (the right way round) into the hand of the laryngoscopist.
Thanks for reading!
Cliff Reid
Resuscitation Doctor, Sydney